1. Miranda, J. J. et al. Understanding the rise of cardiometabolic diseases in low- and middle-income countries. Nat. Med. 25, 1667–1679 (2019).
2. Wang, Y. et al. Has the prevalence of overweight, obesity and central obesity levelled off in the United States? Trends, patterns, disparities, and future projections for the obesity epidemic. Int. J. Epidemiol. 49, 810–823 (2020).
3. Carding, S., Verbeke, K., Vipond, D. T., Corfe, B. M. & Owen, L. J. Dysbiosis of the gut microbiota in disease. Microb. Ecol. Health Dis. 26, 26191 (2015).
4. Rosenbaum, M., Knight, R. & Leibel, R. L. The gut microbiota in human energy homeostasis and obesity. Trends Endocrinol. Metab. 26, 493–501 (2015).
5. Ignacio, A. et al. Correlation between body mass index and faecal microbiota from children. Clin. Microbiol Infect. 22, 258 e251–e258 (2016).
6. Gonzalez, F. J., Jiang, C. & Patterson, A. D. An intestinal microbiota-farnesoid x receptor axis modulates metabolic disease. Gastroenterology 151, 845–859 (2016).
7. San-Cristobal, R., Navas-Carretero, S., Martinez-Gonzalez, M. A., Ordovas, J. M. & Martinez, J. A. Contribution of macronutrients to obesity: implications for precision nutrition. Nat. Rev. Endocrinol. 16, 305–320 (2020).
8. Holmes, E., Li, J. V., Athanasiou, T., Ashrafian, H. & Nicholson, J. K. Understanding the role of gut microbiome-host metabolic signal disruption in health and disease. Trends Microbiol. 19, 349–359 (2011).
9. Spanogiannopoulos, P., Bess, E. N., Carmody, R. N. & Turnbaugh, P. J. The microbial pharmacists within us: a metagenomic view of xenobiotic metabolism. Nat. Rev. Microbiol. 14, 273–287 (2016).
10. Cani, P. D. et al. Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56, 1761–1772 (2007).
11. Cani, P. D. et al. Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57, 1470–1481 (2008).
12. Hoyles, L. et al. Molecular phenomics and metagenomics of hepatic steatosis in non-diabetic obese women. Nat. Med. 24, 1070–1080 (2018).
13. Wang, Z. et al. Gut flora metabolism of phosphatidylcholine promotes cardiovascular disease. Nature 472, 57–63 (2011).
14. Koeth, R. A. et al. Intestinal microbiota metabolism of L-carnitine, a nutrient in red meat, promotes atherosclerosis. Nat. Med. 19, 576–585 (2013).
15. Wikoff, W. R. A. et al. Metabolomics analysis reveals large effects of gut microflora on mammalian blood metabolites. Proc. Natl Acad. Sci. USA 106, 3698–3703 (2009).
16. Peisl, B. Y. L., Schymanski, E. L. & Wilmes, P. Dark matter in host-microbiome metabolomics: tackling the unknowns-a review. Anal. Chim. Acta 1037, 13–27 (2018).
17. Goo, E., An, J. H., Kang, Y. & Hwang, I. Control of bacterial metabolism by quorum sensing. Trends Microbiol. 23, 567–576 (2015).
18. Bajpai, P., Darra, A. & Agrawal, A. Microbe-mitochondrion crosstalk and health: an emerging paradigm. Mitochondrion 39, 20–25 (2018).
19. Donohoe, D. R. et al. The microbiome and butyrate regulate energy metabolism and autophagy in the mammalian colon. Cell Metab. 13, 517–526 (2011).
20. Mollica, M. P. et al. Butyrate regulates liver mitochondrial function, efficiency, and dynamics in insulin-resistant obese mice. Diabetes 66, 1405–1418 (2017).
21. Yardeni, T. et al. Host mitochondria influence gut microbiome diversity: a role for ROS. Sci. Signal. 12, eaaw3159 (2019).
22. Bäckhed, F., Manchester, J. K., Semenkovich, C. F. & Gordon, J. I. Mechanisms underlying the resistance to diet-induced obesity in germ-free mice. Proc. Natl Acad. Sci. USA 104, 979–984 (2007).
23. Bellissimo, M. P. et al. Plasma high-resolution metabolomics differentiates adults with normal weight. Obes. Lean Individ. Obes. 27, 1729–1737 (2019).
24. Cioffi, C. & Vos, M. B. Su1506—comparison of plasma metabolomics profiles of pediatric NASH vs. NAFLD. Gastroenterology 154, S-1161 (2018).
25. Mølstad, P. The efflux of l-carnitine from cells in culture (CCL27). Biochim. Biophys. Acta 597, 166–173 (1980).
26. Nagata, N. et al. Effects of bowel preparation on the human gut microbiome and metabolome. Sci. Rep. 9, 4042 (2019).
27. Ringseis, R., Keller, J. & Eder, K. Role of carnitine in the regulation of glucose homeostasis and insulin sensitivity: evidence from in vivo and in vitro studies with carnitine supplementation and carnitine deficiency. Eur. J. Nutr. 51, 1–18 (2012).
28. Fritz, I. B. Action of carnitine on long chain fatty acid oxidation by liver. Am. J. Physiol. 197, 297–304 (1959).
29. Noland, R. C. et al. Carnitine insufficiency caused by aging and overnutrition compromises mitochondrial performance and metabolic control. J. Biol. Chem. 284, 22840–22852 (2009).
30. Bianchi, P. B. L., Davis, D. C. & Carnitine, A. T. Supplementation ameliorates the steatosis and ketosis induced by pivalate in rats. J. Nutr. 126, 2873–2879 (1996).
31. Asai, T. et al. Combined therapy with PPARalpha agonist and l-carnitine rescues lipotoxic cardiomyopathy due to systemic carnitine deficiency. Cardiovasc. Res. 70, 566–577 (2006).
32. Jiang, F. et al. L-carnitine ameliorates the liver inflammatory response by regulating carnitine palmitoyltransferase I-dependent PPARγ signaling. Mol. Med. Rep. 13, 1320–1328 (2016).
33. Libert, D. M., Nowacki, A. S. & Natowicz, M. R. Metabolomic analysis of obesity, metabolic syndrome, and type 2 diabetes: amino acid and acylcarnitine levels change along a spectrum of metabolic wellness. PeerJ 6, https://doi.org/10.7717/peerj.5410 (2018).
34. Koves, T. R. et al. Mitochondrial overload and incomplete fatty acid oxidation contribute to skeletal muscle insulin resistance. Cell Metab. 7, 45–56 (2008).
35. Spaniol, M. et al. Mechanisms of liver steatosis in rats with systemic carnitine deficiency due to treatment with trimethylhydraziniumpropionate. J. Lipid Res. 44, 144–153 (2003).
36. Karkkainen, O. et al. Diets rich in whole grains increase betainized compounds associated with glucose metabolism. Am. J. Clin. Nutr. 108, 971–979 (2018).
37. Servillo, L. et al. Ruminant meat and milk contain delta-valerobetaine, another precursor of trimethylamine N-oxide (TMAO) like gamma-butyrobetaine. Food Chem. 260, 193–199 (2018).
38. Servillo, L. et al. Carnitine precursors and short-chain acylcarnitines in water buffalo milk. J. Agric. Food Chem. 66, 8142–8149 (2018).
39. Ye, E. Q., Chacko, S. A., Chou, E. L., Kugizaki, M. & Liu, S. Greater whole-grain intake is associated with lower risk of type 2 diabetes, cardiovascular disease, and weight gain. J. Nutr. 142, 1304–1313 (2012).
40. Wang, Y. & Beydoun, M. A. Meat consumption is associated with obesity and central obesity among US adults. Int J. Obes. 33, 621–628 (2009).
41. Li, X. S. et al. Untargeted metabolomics identifies trimethyllysine, a TMAO-producing nutrient precursor, as a predictor of incident cardiovascular disease risk. JCI Insight 3, https://doi.org/10.1172/jci.insight.99096 (2018).
42. Koeth, R. A. et al. gamma-Butyrobetaine is a proatherogenic intermediate in gut microbial metabolism of l-carnitine to TMAO. Cell Metab. 20, 799–812 (2014).
43. Cho, I. et al. Antibiotics in early life alter the murine colonic microbiome and adiposity. Nature 488, 621–626 (2012).
44. Cox, L. M. Antibiotics shape microbiota and weight gain across the animal kingdom. Anim. Front. 6, 8–14 (2016).
45. Stark, C. M., Susi, A., Emerick, J. & Nylund, C. M. Antibiotic and acid-suppression medications during early childhood are associated with obesity. Gut 68, 62–69 (2019).
46. Peters, B. A. et al. A taxonomic signature of obesity in a large study of American adults. Sci. Rep. 8, 9749 (2018).
47. Zhao, M. et al. TMAVA, a metabolite of intestinal microbes, is increased in plasma from patients with liver steatosis, inhibits gamma-butyrobetaine hydroxylase, and exacerbates fatty liver in mice. Gastroenterology 158, https://doi.org/10.1053/j.gastro.2020.02.033 (2020).
48. Sagan, L. On the origin of mitosing cells. J. Theor. Biol. 14, 225–274 (1967).
49. Ristow, M. Unraveling the truth about antioxidants: mitohormesis explains ROS-induced health benefits. Nat. Med. 20, 709–711 (2014).
50. Khan, S. A. et al. ATGL-catalyzed lipolysis regulates SIRT1 to control PGC-1α/PPAR-α signaling. Diabetes 64, 418 (2015).
51. Montagner, A. et al. Liver PPARalpha is crucial for whole-body fatty acid homeostasis and is protective against NAFLD. Gut 65, 1202–1214 (2016).
52. Azevedo, R. A. & Arruda, P. High-lysine maize: the key discoveries that have made it possible. Amino Acids 39, 979–989 (2010).
53. Torre, D., Lachmann, A. & Ma’ayan, A. BioJupies: automated generation of interactive notebooks for RNA-seq data analysis in the cloud. Cell Syst. 7, 556–561.e553 (2018).
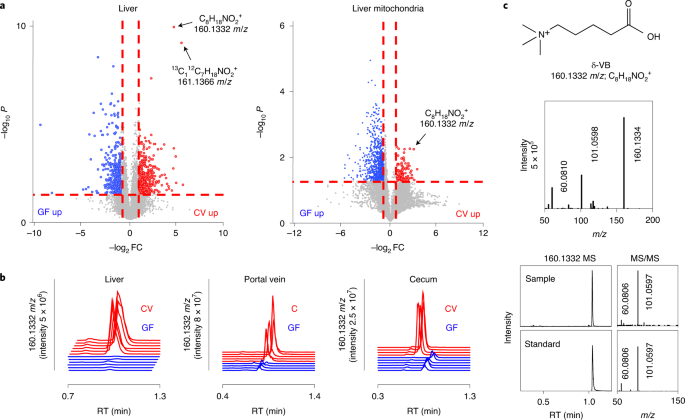
54. Go, Y. M. et al. Mitochondrial metabolomics using high-resolution Fourier-transform mass spectrometry. Methods Mol. Biol. 1198, 43–73 (2014).
55. Liu, K. H. et al. High-resolution metabolomics assessment of military personnel: evaluating analytical strategies for chemical detection. J. Occup. Environ. Med. 58, S53–S61 (2016).
56. Liu, K. H. et al. Reference standardization for quantification and harmonization of large-scale metabolomics. Anal. Chem. https://doi.org/10.1021/acs.analchem.0c00338 (2020).
57. Yu, T. & Jones, D. P. Improving peak detection in high-resolution LC/MS metabolomics data using preexisting knowledge and machine learning approach. Bioinformatics 30, 2941–2948 (2014).
58. Yu, T., Park, Y., Johnson, J. M. & Jones, D. P. apLCMS–adaptive processing of high-resolution LC/MS data. Bioinformatics 25, 1930–1936 (2009).
59. Uppal, K. et al. xMSanalyzer: automated pipeline for improved feature detection and downstream analysis of large-scale, non-targeted metabolomics data. BMC Bioinf. 14, 15 (2013).
60. Ritchie, M. E. et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 43, e47–e47 (2015).
61. Li, S. et al. Predicting network activity from high throughput metabolomics. PLoS Comput. Biol. 9, e1003123 (2013).
62. Uppal, K., Walker, D. I. & Jones, D. P. xMSannotator: an R package for network-based annotation of high-resolution metabolomics data. Anal. Chem. 89, 1063–1067 (2017).
63. Smith, C. A. et al. METLIN: a metabolite mass spectral database. Ther. Drug Monit. 27, 747–751 (2005).
64. Tars, K. et al. Targeting carnitine biosynthesis: discovery of new inhibitors against γ-butyrobetaine hydroxylase. J. Med. Chem. 57, 2213–2236 (2014).
65. Chen, C. M. F. & Leo Benoiton, N. A new method of quaternizing amines and its use in amino acid and peptide chemistry. Can. J. Chem. 54, 3310 (1976).
66. R Core Team. R: A Language Environment for Statistical Computing (R Foundation for Statistical Computing, 2014); https://www.R-project.org/
67. Rask, K. J., Brigham, K. l., Fau-Johns, M. M. E. & Johns, M. M. Integrating comparative effectiveness research programs into predictive health: a unique role for academic health centers. Acad. Med. 86, 718–723 (2011).
68. Brigham, K. L. Predictive health: the imminent revolution in health care. J. Am. Geriatr Soc. 58, S298–S302 (2010).
69. Soltow, Q. A. et al. High-performance metabolic profiling with dual chromatography-Fourier-transform mass spectrometry (DC-FTMS) for study of the exposome. Metabolomics 9, 132–143 (2011).
https://www.nature.com/articles/s42255-021-00502-8