1.WHO cov-19 interactive timeline (accessed 19 April 2021); https://www.who.int/emergencies/diseases/novel-coronavirus-2019/interactive-timeline2.JHU cov-19 map. (accessed 19 April 2021); https://coronavirus.jhu.edu/map.html3.OWID data on the coronavirus pandemic. https://ourworldindata.org/mortality-risk-covid4.Flint, S. & Tahrani, A. Covid-19 and obesity-lack of clarity, guidance, and implications for care. Lancet Diabetes Endocrinol. 8, 474–475 (2020).CAS PubMed PubMed Central Google Scholar 5.Zhou, Y., Chi, J., Lv, W. & Wang, Y. Obesity and diabetes as high-risk factors for severe coronavirus disease 2019 (covid-19). Diabetes Metab. Res. Rev. 37, e3377 (2021).CAS PubMed Google Scholar 6.Richardson, S. et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with covid-19 in the new york city area. JAMA 323, 2052–2059 (2020).CAS PubMed PubMed Central Google Scholar 7.Zaki, N., Alashwal, H. & Ibrahim, S. Association of hypertension, diabetes, stroke, cancer, kidney disease, and high-cholesterol with covid-19 disease severity and fatality: A systematic review. Diabetes Metab. Syndr. 14, 1133–1142 (2020).PubMed PubMed Central Google Scholar 8.Ji, Y., Ma, Z., Peppelenbosch, M. P. & Pan, Q. Potential association between covid-19 mortality and health-care resource availability. Lancet Glob. Health 8, e480 (2020).PubMed PubMed Central Google Scholar 9.Kenyon, C. Flattening-the-curve associated with reduced covid-19 case fatality rates- an ecological analysis of 65 countries. J. Infect. 81, e98–e99 (2020).CAS PubMed PubMed Central Google Scholar 10.Dowd, J. B. et al. Demographic science aids in understanding the spread and fatality rates of covid-19. PNAS 117, 9696–9698 (2020).CAS PubMed PubMed Central Google Scholar 11.Hou, Y. J. et al. Sars-cov-2 reverse genetics reveals a variable infection gradient in the respiratory tract. Cell 182, 429-446.e14 (2020).CAS PubMed PubMed Central Google Scholar 12.Zhang, X. et al. Viral and host factors related to the clinical outcome of covid-19. Nature 583, 437–440 (2020).ADS CAS PubMed Google Scholar 13.Di Maria, E., Latini, A., Borgiani, P. & Novelli, G. Genetic variants of the human host influencing the coronavirus-associated phenotypes (sars, mers and covid-19): Rapid systematic review and field synopsis. Human Genom. 14, 1–19 (2020). Google Scholar 14.Zeberg, H. & Pääbo, S. The major genetic risk factor for severe covid-19 is inherited from neanderthals. Nature 587, 610–612 (2020).ADS CAS PubMed Google Scholar 15.Oksanen, A. et al. Month follow-up study on covid-19 mortality in 25 european countries. JMIR Public Health Surv. 6, e19218 (2020). Google Scholar 16.MacLean, O. A., Orton, R. J., Singer, J. B. & Robertson, D. L. No evidence for distinct types in the evolution of sars-cov-2. Virus Evol. 6, veaa034 (2020).PubMed PubMed Central Google Scholar 17.Halley, J. M., Vokou, D., Pappas, G. & Sainis, I. Sars-cov-2 mutational cascades and the risk of hyper-exponential growth. Microb. Pathog. 161, 105237 (2021).CAS PubMed PubMed Central Google Scholar 18.Ellinghaus, D. et al. Genome wide association study of severe covid-19 with respiratory failure. N. Engl. J. Med. 283, 1522–34 (2020). Google Scholar 19.Pairo-Castineira, E. et al. Genetic mechanisms of critical illness in covid-19. Nature 591, 92–98 (2021).ADS PubMed Google Scholar 20.Guilger-Casagrande, M., de Barros, C. T., Antunes, V. A. N., de Araujo, D. R. & Lima, R. Perspectives and challenges in the fight against covid-19: The role of genetic variability. Front Cell Infect. Microbiol. 11, 598875 (2021).PubMed PubMed Central Google Scholar 21.Wickenhagen, A. et al. A prenylated dsrna sensor protects against severe covid-19. Science 374, eabj3624 (2021).CAS PubMed Google Scholar 22.Escobar, L. E., Molina-Cruz, A. & Barillas-Mury, C. Bcg vaccine protection from severe coronavirus disease 2019 (covid-19). PNAS 117, 17720–17726 (2020).CAS PubMed PubMed Central Google Scholar 23.Fu, W. et al. Reconcile the debate over protective effects of bcg vaccine against covid-19. Sci. Rep. 11, 8356 (2021).CAS PubMed PubMed Central Google Scholar 24.Chimoyi, L. et al. An ecological study to evaluate the association of bacillus calmette-guerin (bcg) vaccination on cases of sars-cov2 infection and mortality from covid-19. PLoS One 15, e0243707 (2020).CAS PubMed PubMed Central Google Scholar 25.Li, W. X. Worldwide inverse correlation between bacille calmette-guérin (bcg) immunization and covid-19 mortality. Infection 49, 463–473 (2021).CAS PubMed Google Scholar 26.Bowe, B. et al. Ambient fine particulate matter air pollution and the risk of hospitalization among covid-19 positive individuals: Cohort study. Environ. Int. 154, 106564 (2021).CAS PubMed PubMed Central Google Scholar 27.Travaglio, M. et al. Links between air pollution and covid-19 in england. Environ. Pollut. 268, 115859 (2021).CAS PubMed PubMed Central Google Scholar 28.Cazzolla Gatti, R., Velichevskaya, A., Tateo, A., Amoroso, N. & Monaco, A. Machine learning reveals that prolonged exposure to air pollution is associated with sars-cov-2 mortality and infectivity in italy. Environ. Pollut. 267, 115471 (2020).CAS PubMed PubMed Central Google Scholar 29.Cassan, G. & Van Steenvoort, M. Political regime and covid 19 death rate: Efficient, biasing or simply different autocracies? An econometric analysis. SSM Popul. Health 16, 100912 (2021).PubMed PubMed Central Google Scholar 30.Blood type distribution by country. (accessed 16 January 2021); https://en.wikipedia.org/wiki/Blood_type_distribution_by_country31.The complete our world in data covid-19 dataset. (accessed 16 January 2021); https://github.com/owid/covid-19-data/tree/master/public/data32.Biau, G. Analysis of a random forests model. J. Mach. Learn. Res. 13, 1063–1095 (2012).MathSciNet MATH Google Scholar 33.Kursa, M. B. & Rudnicki, W. R. Feature selection with the boruta package. J. Stat. Softw. 36, 1–13 (2010). Google Scholar 34.Kursa, M. B., Jankowski, A. & Rudnicki, W. R. Boruta: A system for feature selection. Fundam. Inform. 101, 271–285 (2010).MathSciNet Google Scholar 35.Breiman, L. Random forests. Mach. Learn. 45, 32–45 (2001).MATH Google Scholar 36.R Core Team. R: A Language and Environment for Statistical Computing. R Foundation for Statistical Computing, Vienna, Austria (2020). https://www.R-project.org/37.Kruskal, W. H. & Wallis, W. A. Use of ranks in one-criterion variance analysis. J. Am. Stat. Assoc. 47, 583–621 (1952).MATH Google Scholar 38.Shelton, J. F. et al. Trans-ethnic analysis reveals genetic and non-genetic associations with covid-19 susceptibility and severity. medRxiv (2020).39.Zhao, J. et al. Relationship between the abo blood group and the covid-19 susceptibility. Clin. Infect. Dis. 73, ciaa1150 (2020). Google Scholar 40.Wu, Y., Feng, Z. P. L. & Yu, Q. Relationship between the abo blood group and the covid-19 susceptibility. Clin. Chim. Acta 509, 220–3 (2020).CAS PubMed PubMed Central Google Scholar 41.Ray, J. G., Schull, M. J., Vermeulen, M. J. & Park, A. L. Association between abo and rh blood groups and sars-cov-2 infection or severe covid-19 illness: A population-based cohort study. Ann. Int. Med. 174, 308–315 (2021).PubMed Google Scholar 42.Zietz, M., Zucker, J. & Tatonetti, N. P. Associations between blood type and covid-19 infection, intubation, and death. Nat. Commun. 11, 5761 (2020).ADS CAS PubMed PubMed Central Google Scholar 43.HernandézCordero, A. I. E. A. Multi-omics highlights abo plasma protein as a causal risk factor for covid-19. Hum. Genet. 140, 969–979 (2021). Google Scholar 44.Valenti, L. et al. Association of abo blood group and secretor phenotype with severe covid-19. Transfusion 60, 3067–3070 (2020).CAS PubMed Google Scholar 45.Horowitz, J. E. et al. Genome-wide analysis in 756,646 individuals provides first genetic evidence that ace2 expression influences covid-19 risk and yields genetic risk scores predictive of severe disease. medRxiv [Preprint] (2021).46.Guillon, P. et al. Inhibition of the interaction between the sars-cov spike protein and its cellular receptor by anti-histo-blood group antibodies. Glycobiology 18, 1085–1093 (2008).CAS PubMed Google Scholar 47.Deleers, M. et al. Covid-19 and blood groups: Abo antibody levels may also matter. Int. J. Infect Dis. 104, 242–249 (2021).CAS PubMed Google Scholar 48.Pendu, J. L., Breiman, A., Rocher, J., Dion, M. & Ruvoen-Clouet, N. Abo blood types and covid-19: Spurious, anecdotal, or truly important relationships? A reasoned review of available data. Viruses 13, 160 (2021).PubMed PubMed Central Google Scholar 49.Wu, B. B., Gu, D. Z., Yu, J. N., Yang, J. & Shen, W. Q. Association between abo blood groups and covid-19 infection, severity and demise: A systematic review and meta-analysis. Infect. Genet. Evol. 84, 104485 (2020).CAS PubMed PubMed Central Google Scholar 50.Liu, Y., Haussinger, L., Steinacker, J. M. & Dinse-Lambracht, A. Association between the dynamics of the covid-19 epidemic and abo blood type distribution. Epidemiol. Infect. 149, e19 (2021).CAS PubMed Google Scholar 51.Ellis, P. J. I. Modelling suggests abo histo-incompatibility may substantially reduce sars-cov-2 transmission. Epidemics 35, 100446 (2021).PubMed PubMed Central Google Scholar 52.Miotto, M., Di Rienzo, L., Gosti, G., Milanetti, E. & Ruocco, G. Does blood type affect the covid-19 infection pattern?. PLoS One 16, e0251535 (2021).CAS PubMed PubMed Central Google Scholar 53.Stowell, S. R. & Stowell, C. P. Biologic roles of the abh and lewis histo-blood group antigens part ii: Thrombosis, cardiovascular disease and metabolism. Vox Sang 114, 535–552 (2019).PubMed Google Scholar 54.Trégouët, D. A. et al. Common susceptibility alleles are unlikely to contribute as strongly as the fv and abo loci to vte risk: Results from a gwas approach. Blood 113, 5298–303 (2009).PubMed Google Scholar 55.Paré, G. et al. Novel association of abo histo-blood group antigen with soluble icam-1: Results of a genome wide association study of 6,578 women. PLoS Genet. 4, e1000118 (2008).PubMed PubMed Central Google Scholar 56.Frischmuth, T. et al. Joint effect of multiple prothrombotic genotypes and obesity on the risk of incident venous thromboembolism. Thromb Haemost. (2021).57.Skille, H. et al. Combined effects of five prothrombotic genotypes and cancer on the risk of a first venous thromboembolic event. J. Thromb Haemost. 18, 2861–2869 (2020).CAS PubMed Google Scholar 58.Sejrup, J. K. et al. Myocardial infarction, prothrombotic genotypes, and venous thrombosis risk: The tromsø study. Res. Pract. Thromb Haemost. 4, 247–254 (2020).CAS PubMed PubMed Central Google Scholar 59.Groot, H. E. et al. Genetically determined abo blood group and its associations with health and disease. Arterioscler. Thromb Vasc. Biol. 40, 830–838 (2020).CAS PubMed Google Scholar 60.Sabater-Lleal, M. E. A. Genome-wide association transethnic meta-analyses identifies novel associations regulating coagulation factor viii and von willebrand factor plasma levels. Circulation 139, 620–635 (2019).CAS PubMed PubMed Central Google Scholar 61.Timmann, C. et al. Genome-wide association study indicates two novel resistance loci for severe malaria. Nature 489, 443–446 (2012).ADS CAS PubMed Google Scholar 62.Band, G. et al. Malaria genomic epidemiology network: Insights into malaria susceptibility using genome-wide data on 17,000 individuals from africa, asia and oceania. Nat. Commun. 10, 5732 (2019).ADS Google Scholar 63.Heit, J. A. et al. A genome-wide association study of venous thromboembolism identifies risk variants in chromosomes 1q24.2 and 9q. J. Thromb. Haemostasis: JTH 10, 1521–1531 (2012).CAS Google Scholar 64.Dahlén, T., Clements, M., Zhao, J., Olsson, M. L. & Edgren, G. An agnostic study of associations between abo and rhd blood group and phenome-wide disease risk. Elife 10, e65658 (2021).PubMed PubMed Central Google Scholar 65.Souilmi, Y. et al. An ancient viral epidemic involving host coronavirus interacting genes more than 20,000 years ago in east asia. bioRxiv (2021).66.Patella, V., Delfino, G., Bruzzese, D., Giuliano, A. & Sanduzzi, A. The bacillus calmette-guérin vaccination allows the innate immune system to provide protection from severe covid-19 infection. PNAS 117, 25205–25206 (2020).CAS PubMed PubMed Central Google Scholar 67.Klinger, D., Blass, I., Rappoport, N. & Linial, M. Significantly improved covid-19 outcomes in countries with higher bcg vaccination coverage: A multivariable analysis. Vaccines 8, 523 (2020). Google Scholar 68.Brooks, N. A. E. A. The association of coronavirus disease-19 mortality and prior bacille calmette-guerin vaccination: A robust ecological analysis using unsupervised machine learning. Sci. Rep. 11, 1–9 (2021). Google Scholar Page 2 Genetic features Demographic indicators Medical indicators Economic indicators Life style indicators O+ A+ B+ AB+ O− A− B− AB− O/non O Rh−/Rh+ Population density Life expectancy at birth GDP per capita Percentage of female smokers Median age of the population Cardiovascular death rate Total healthcare expenditure Percentage of male smokers Population aged 65 or older Diabetes prevalence Hospital beds per thousand inhabitants Population aged 70 or older We used five kinds of features: genetic, demographic, economic, medical, and life style indicators.
https://www.nature.com/articles/s41598-021-04162-2
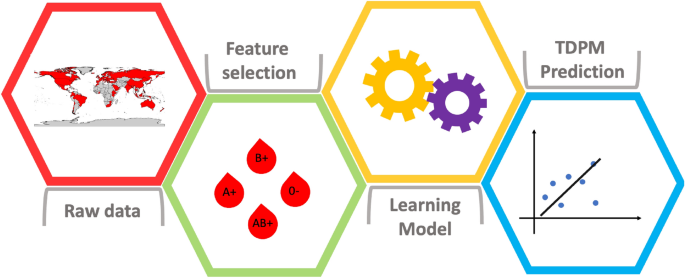
Country-level factors dynamics and ABO/Rh blood groups contribution to COVID-19 mortality